Healthcare leaders face a unique paradox. While revenue is often stabilizing, operating margins remain razor-thin, driven by rising labor costs and complex reimbursement models. In this environment, a static PDF document stored on a shared drive is shelfware rather than strategy. To drive true organizational growth, leaders need dynamic, reference-ready blueprints that connect high-level vision to daily action.
This article provides a definitive gallery of examples of strategic plans in hospitals and health systems. We will move beyond theory to examine four specific, proven strategic frameworks from system-wide financial goals to clinic-level efficiency. You will learn how to transform static planning documents into living, trackable execution frameworks that link departmental initiatives to organizational outcomes.
In This Article
- Key Components of a Health System Strategic Plan
- Real-World Strategic Plan Examples
- Hospital Strategic Planning Challenges and Solutions
- The Operating System for Healthcare Strategy
- Frequently Asked Questions About Hospital Strategic Planning
Key Components of a Health System Strategic Plan
Before exploring the specific blueprints, we must establish the essential structural elements that allow a plan to be measurable. A truly effective health system strategic plan demands a mechanical structure that links vision to accountability.

Vision, Mission and Core Values
Your vision is the destination. It is the North Star that guides decision-making when the market is foggy. Successful plans anchor every initiative back to these core tenets, whether that is delivering compassionate care to underserved individuals or becoming the regional leader in neurological outcomes. If a strategic initiative does not align with the mission, do not include it in the plan.
Strategic Priorities
The most common mistake in hospital planning is the laundry list approach. Effective plans narrow their focus to three to five overarching priority areas, often referred to as pillars. Common examples include:
- Financial stewardship
- Patient safety
- Workforce excellence
- Community growth
These pillars serve as the supports that organize all subsequent activity.
Metrics and KPIs
Vague goals like “improve culture” are impossible to track. Progressive plans use hard metrics to define success. Instead of “improve retention,” a valid key performance indicator (KPI) is “reduce RN turnover by 15% by Q4.” These metrics must be quantifiable, time-bound and accessible to leadership in real time.
Initiatives and Action Plans
Initiatives are the specific projects designed to move the needle on your KPIs. Crucially, every initiative must have a single assigned owner. Shared ownership often leads to a lack of accountability.
Managing these components in spreadsheets leads to version control nightmares and fragmented data. Healthcare strategic management platforms digitally organize these elements, directly linking vision and mission to specific action plans. The result is instant visibility into what is working and what is at risk.
Real-World Strategic Plan Examples
The following section outlines four distinct strategic blueprints with specific details on how to create a hospital strategic plan. They are designed to be adapted to your specific organizational needs, ranging from broad system-wide plans to focused departmental strategies.
Blueprint 1: The Comprehensive Hospital Strategic Plan
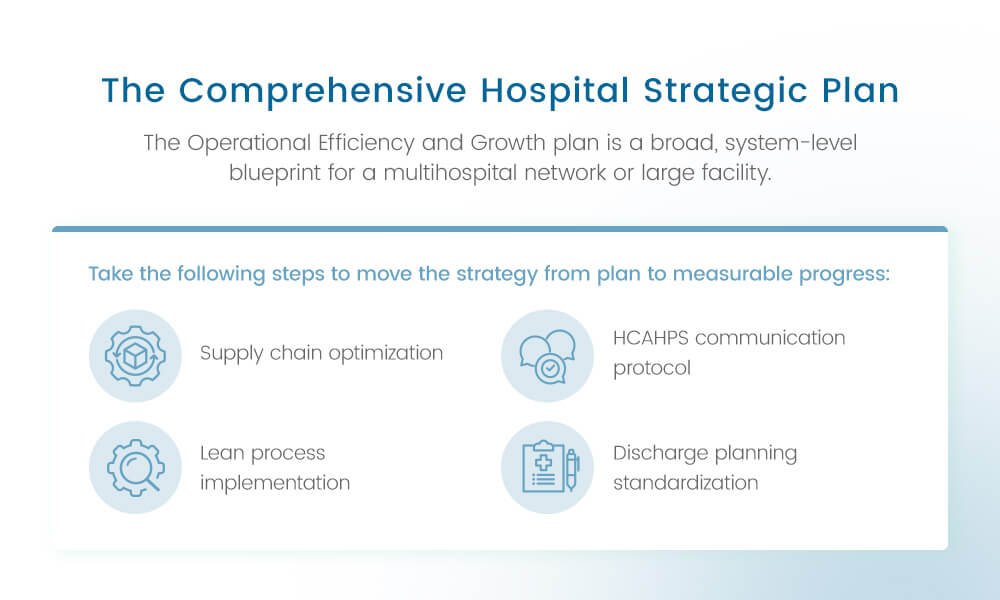
The Operational Efficiency and Growth plan is a broad, system-level blueprint for a multihospital network or large facility. The primary drivers are financial sustainability and core service strength.
According to the American Hospital Association (AHA) 2026 Environmental Scan, financial headwinds persist as hospitals face continued pressure from high labor costs, inflation and reimbursement challenges. While a stabilization trend is evident, managing expenses remains a top priority for leaders. This blueprint addresses that reality by striking a balance between fiscal discipline and the patient experience.
- Primary goal: Achieve a 15% reduction in non-labor operational costs and enhance Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) patient satisfaction scores by 20% in three years.
- Pillars and strategies: For financial stewardship, focus on lean process improvement, supply chain optimization and revenue cycle management. For patient experience, prioritize staff communication training, facility upgrades and patient flow management.
- Metrics and KPIs: Track cost per adjusted patient day, net operating margin, HCAHPS Likelihood to Recommend and throughput/discharge efficiency.
- Execution gap risk: Tracking cross-departmental initiatives, like a Lean project that intersects with supply chain and clinical nursing, is notoriously difficult. A unified platform ensures that financial savings in the supply chain do not negatively impact patient outcomes, linking data points that usually sit in silos.
Take the following steps to move the strategy from plan to measurable progress:
- Supply chain optimization: Conduct a system-wide audit of high-cost items to identify areas for improvement. Establish a Value Analysis Committee to vet all new equipment and standardize vendor contracts to reduce variance in preference cards in the operating room (OR).
- Lean process implementation: Launch a six-month initiative to map the patient journey from admission to discharge. The goal is to identify three major sources of waste, such as redundant documentation or delays in patient transport.
- HCAHPS communication protocol: Adherence to safety and communication standards is critical. The Joint Commission’s 2026 National Patient Safety Goalsexplicitly highlight Goal NPSG.02.03.01, emphasizing the need to deliver important test results to the right staff member on time. To support this, implement mandatory scenario-based training for all clinical staff to standardize how information is conveyed to patients and colleagues.
- Discharge planning standardization: Formalize a Discharge Huddle process that begins within 24 hours of admission. This process coordinates follow-up care early, reducing length of stay (LOS) and readmission risk.
Blueprint 2: The Focused Hospital Nursing Strategic Plan

The Workforce Excellence and Quality plan is a departmental strategy that is crucial for patient care quality, talent retention and achieving or maintaining Magnet® Recognition from the American Nurses Credentialing Center (ANCC).
Retention remains a strategic imperative. The American Nurses Association 2025 Membership Assembly prioritized workforce sustainability and the ethical integration of AI to reduce administrative burden. This blueprint operationalizes those recommendations, moving beyond basic staffing to focus on role clarity and advanced support systems.
- Primary goal: Reduce nurse turnover by 15% and increase the percentage of Bachelor of Science in Nursing (BSN)-prepared nurses to 80% in two years.
- Pillars and strategies: For workforce excellence, focus on recruitment pipeline development, tuition reimbursement, mentorship programs and improved staffing ratios. For nursing practice and education, implement a Magnet®-aligned strategic planning framework for clinics and hospitals, invest in simulation training and standardize clinical protocols.
- Metrics and KPIs: RN turnover rate, time to fill open positions, BSN-prepared % of staff, patient pain management scores and nurse-to-patient communication frequency.
- Execution gap risk: Monitoring soft goals, such as mentorship engagement, is critical for achieving hard outcomes, like retention. Use a technology solution that empowers leadership to track execution of retention initiatives and correlate that activity with turnover rates in real time.
These steps are crucial for moving the needle from strategies to recorded metrics that serve the primary goal:
- Retention program launch: Formalize a new graduate nurse residency program with assigned mentors. Mandate 90-day check-ins by nurse managers to catch burnout early. Track these touchpoints via your execution software.
- Education incentive program: Increase the tuition reimbursement cap for BSN and Master of Science in Nursing (MSN) programs. Create a transparent clinical ladder that ties salary increases directly to certification and further education.
- Staffing ratio review: Conduct a unit-by-unit analysis of staffing ratios against industry best practices. Develop a phased plan to adjust staffing to meet target ratios on high-acuity units.
- Shared governance implementation: Form unit-level Shared Governance Councils with the authority to propose and implement changes related to clinical practice and the work environment.
Blueprint 3: The Integrated Health System Strategic Plan
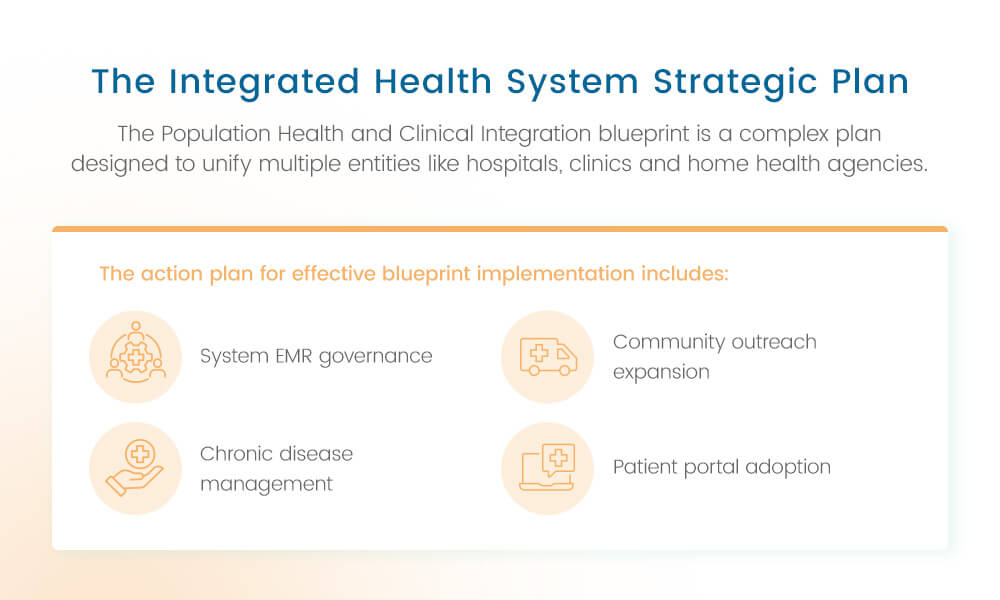
The Population Health and Clinical Integration blueprint is a complex plan designed to unify multiple entities like hospitals, clinics and home health agencies. This blueprint focuses on standardization and community impact.
Integration efficiency is a major hurdle for U.S. health systems. The Commonwealth Fund’s Mirror, Mirror 2024 report indicates that administrative efficiency in the U.S. lags behind that of peer nations. This blueprint tackles that inefficiency by driving standardization across the continuum of care.
- Primary goal: Achieve system-wide standardization of emergency medical responder (EMR) protocols and reduce community readmission rates for two major chronic diseases by 10%.
- Pillars and strategies: For clinical integration, standardize EMR templates and protocols across all system sites. For population health, expand community outreach by launching system-wide chronic disease management programs and increasing preventive care screenings. For digital transformation, implement a single, integrated patient portal and telehealth platform that spans the entire system.
- Metrics and KPIs: Percentage of protocols standardized, readmission rates for heart failure and chronic obstructive pulmonary disease (COPD), telehealth utilization rate and community health survey results.
- Execution gap risk: This plan involves hundreds of stakeholders across different facilities. Implement a system that provides a single, executive-level view of integration progress. A single viewpoint is essential for managing complex interdependencies where a delay in EMR standardization can stall population health initiatives.
The action plan for effective blueprint implementation includes:
- System EMR governance: Establish a Clinical Standardization Task Force comprising leaders from all hospitals and clinics. Prioritize the top 10 most common clinical pathways, like sepsis and stroke, for immediate standardization.
- Chronic disease management: Launch a Transition of Care team to follow high-risk patients for 30 days post-discharge, including home health coordination and follow-up telehealth visits.
- Community outreach expansion: Deploy two mobile clinics to underserved areas on a set schedule. Partner with local organizations to host quarterly health screening fairs.
- Patient portal adoption: Roll out a system-wide communication campaign with clear training materials to promote patient registration and usage of the integrated portal.
Blueprint 4: The Agile Ambulatory Care or Clinic Strategic Plan
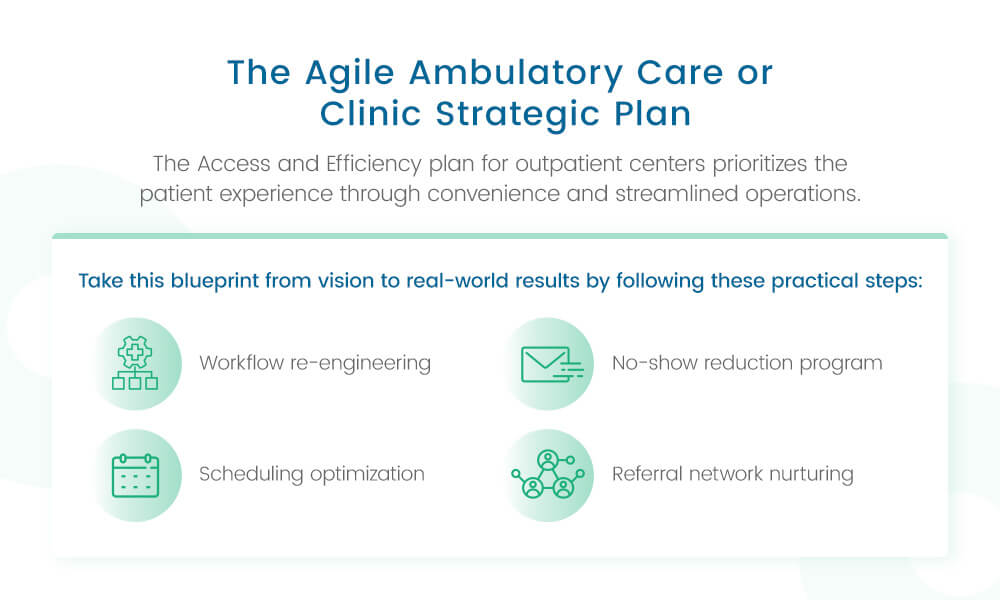
The Access and Efficiency plan for outpatient centers prioritizes the patient experience through convenience and streamlined operations.
The shift away from inpatient care is accelerating. KFF’s Key Facts About Hospitals data confirms the long-term trend of a decrease in inpatient days, alongside a rise in outpatient volume. To capture this volume, clinics must operate with high agility and accessibility.
- Primary goal: Reduce average patient wait times to under 15 minutes and expand specialty service line volume by 30% in two years.
- Pillars and strategies: For access and convenience, implement a new patient check-in system, expand weekend/evening hours and optimize physician scheduling templates. For service line growth, target marketing to primary care provider (PCP) referral networks, recruit specialists, and invest in new equipment.
- Metrics and KPIs: Track average wait time from door to physician, no-show rates, new patient acquisition, and service line volume and revenue.
- Execution gap risk: Clinic managers need real-time data to spot bottlenecks. Advanced dashboards visualize access and efficiency KPIs for each clinic, ensuring rapid course correction on operational initiatives before they impact monthly revenue.
Take this blueprint from vision to real-world results by following these practical steps:
- Workflow re-engineering: Implement a self-check-in kiosk system or digital preregistration. Conduct a time-motion study on clinical flow to eliminate delays between check-in and rooming.
- Scheduling optimization: Analyze appointment length and buffer times for the top three service lines. Adjust scheduling templates to better align with demand and physician workflow.
- No-show reduction program: Implement automated text/email appointment reminders 48 and 24 hours in advance. Launch a policy to call all no-show patients within two hours to reschedule.
- Referral network nurturing: Assign a physician liaison to conduct monthly outreach meetings with the top 10 external PCP practices to review service offerings and referral protocols.
Hospital Strategic Planning Challenges and Solutions
Why do highly paid consultants and brilliant executives still produce plans that fail? The answer lies in the execution gap. Consolidating the takeaways from the blueprints reveals three specific traps that derail even the most well-funded hospital strategies.
Trap 1: The Alignment Gap
Successful plans cannot exist in a vacuum. In a healthy system, the Workforce Excellence and Quality plan is a critical part of the Operational Efficiency and Growth plan by reducing reliance on expensive contract labor. When these plans are disconnected, departments inadvertently work against each other. Finance cuts the training budget to save money, while nursing sees a spike in turnover.
You can address this challenge by visualizing the golden thread that connects daily departmental tasks to high-level organizational pillars.
Trap 2: The Agility Gap
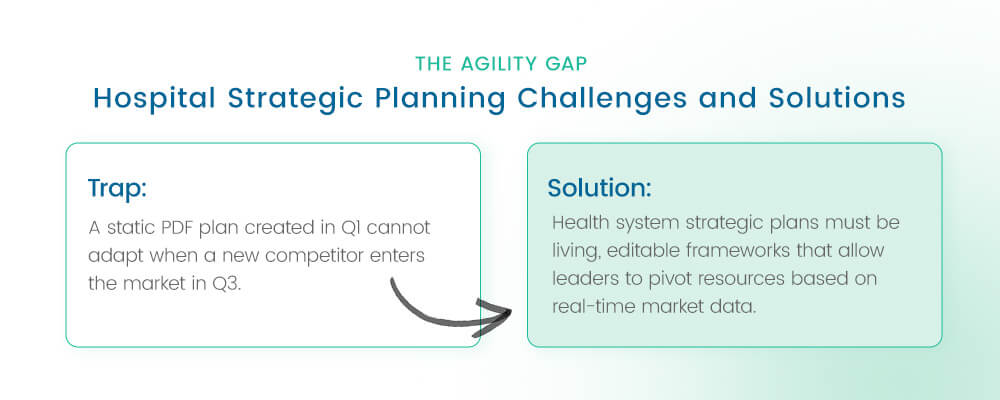
Healthcare is volatile. A static PDF plan created in Q1 cannot adapt when a new competitor enters the market in Q3 or a regulatory change shifts reimbursement models. If your plan is locked in a document, it is already obsolete.
Health system strategic plans must be living, editable frameworks that allow leaders to pivot resources based on real-time market data, rather than relying on annual review cycles.
Trap 3: The Accountability Gap
The primary reason strategic plans fail is a lack of clear ownership. When a plan sits on a shared drive, initiatives lose momentum because no one updates them. “We’ll review it next month” becomes the enemy of progress. Those in charge of executing a hospital’s strategic plan often do not know who to ask for initiative updates, or there are too many people to ask. To become proactive and accelerate execution, strategy leaders must create a system for clear accountability.
Visibility drives accountability. If you can’t see the status of an initiative in real time, it is likely already failing. Many great ideas falter because there is no clear way to keep people and projects on track. Using an automated platform ensures accountability and improves visibility into performance and execution.
The Operating System for Healthcare Strategy
The era of managing billion-dollar health systems with spreadsheets is over. The landscape of strategic planning is evolving from consultant-led, static exercises to self-sustaining, data-driven processes. Leaders are increasingly turning to dedicated platforms to manage this complexity.
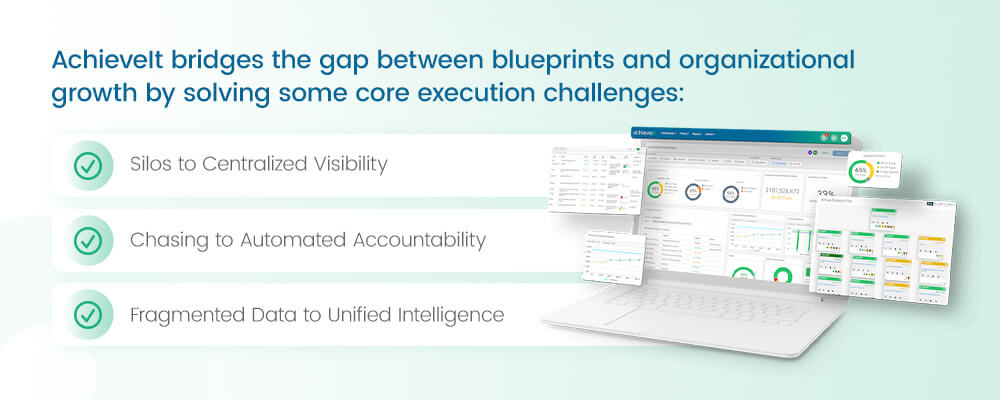
AchieveIt bridges the gap between blueprints and organizational growth by solving some core execution challenges:
Silos to Centralized Visibility
AchieveIt consolidates all strategic plans — from the system-wide view to the specific clinic view — into a single, transparent source of truth. This control-tower view allows executives to drill down from a high-level goal like Financial Health directly into the specific nursing initiatives driving it. You see the status of every initiative in red, yellow or green instantly, without waiting for a quarterly slide deck.
Chasing to Automated Accountability
The platform eliminates the manual drudgery of chasing updates. Instead of a project manager spending time each week emailing staff for status reports, AchieveIt automatically notifies goal owners when updates are due. It ensures that accountability is baked into the workflow, not added as an afterthought.
Fragmented Data to Unified Intelligence
AchieveIt uses centralized dashboards to merge siloed operational data into a clear strategic picture. You can now view HR retention statistics alongside finance margin statistics. This unified view provides the holistic context needed to make informed, agile decisions.
The AchieveIt Advantage
Hospital strategic plans are about tracking tasks, but more importantly, they are about building a culture of execution. By providing a single digital home for your strategy, AchieveIt makes sure that your North Star serves as the daily guide for every decision made across your healthcare system.
Frequently Asked Questions About Hospital Strategic Planning
More of your strategic planning and execution questions answered.
What is the role of a hospital authority strategic plan?
A hospital authority strategic plan differs slightly from a standard private hospital plan because it must account for public funding, regulatory oversight and broader community health mandates. These plans often serve as a contract with the community, detailing how public resources will be used to improve population health outcomes.
Unlike a private system that might prioritize market share, a hospital authority plan focuses heavily on access, equity and the sustainability of essential safety-net services. The Population Health and Clinical Integration plan serves as a strong foundation for this. It emphasizes community outreach and standardized care protocols that are critical for public health authorities.
How do you create a nursing education strategic plan?
A nursing education plan is a subcomponent of the broader workforce strategy. It specifically addresses the build vs. buy talent challenge. Rather than relying solely on expensive recruitment, this plan focuses on upskilling current staff. Key elements typically include:
- Identifying gaps in specialty skills, like those required in an intensive care unit (ICU) or OR, for example.
- Formalizing relationships with local universities to streamline RN-to-BSN pathways.
- Budgeting for high-fidelity simulation labs to accelerate new graduate competency.
- Creating a clear pathway for bedside nurses to transition into management roles, ensuring your educational investments directly support the organization’s long-term clinical quality goals.
Is there a standard strategic nursing department template?
While every organization is unique, a robust strategic plan for a nursing department should ideally include four core quadrants:
- Workforce and culture: This quadrant includes retention rates, engagement scores and shared governance participation.
- Clinical quality: Track HCAHPS scores, infection rates like central line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTI), and patient safety indicators.
- Financial stewardship: This category includes overtime management, supply costs and productivity per unit of service.
- Professional development: Monitor certification rates and educational advancement. Using a standardized template, like the Workforce Excellence and Quality plan, ensures that your nursing leadership is tracking the same North Star metrics as the rest of the executive team. Having the same goals prevents the department from becoming a silo.
Mastering Execution for Organizational Growth
Planning is the blueprint, but execution is the structure that brings it to life. The path to sustainable organizational growth in healthcare requires moving past static documents to dynamic, measurable execution.
By adopting frameworks like the ones outlined above — and supporting them with the right technology — leaders can ensure their strategies result in better patient care, financial health and workforce stability.
Start planning to execute. Request your demo today to see how AchieveIt can bring your hospital’s strategic plans to life.



